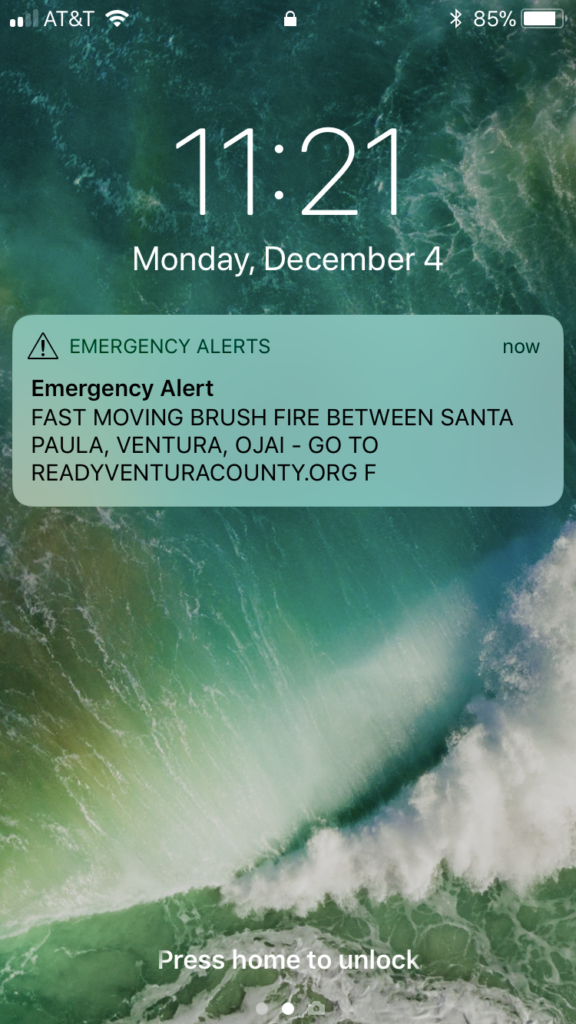
Today we watch the outbreak known as COVID-19 continue to grow with ferocity, spurring emergency proclamations from more than half of the United States. The number of Emergency Operations Centers active in California softly escalates to what is likely an all-time high since my career in emergency management began. The scale of impacts the COVID-19 virus will have on our society remains to be seen, yet there are already some salient lessons that can be gleaned from this experience. These are my thoughts so far as my world is slowly consumed by the first pandemic of my emergency management career.

Social Distancing, Telework and Disproportionate Impacts
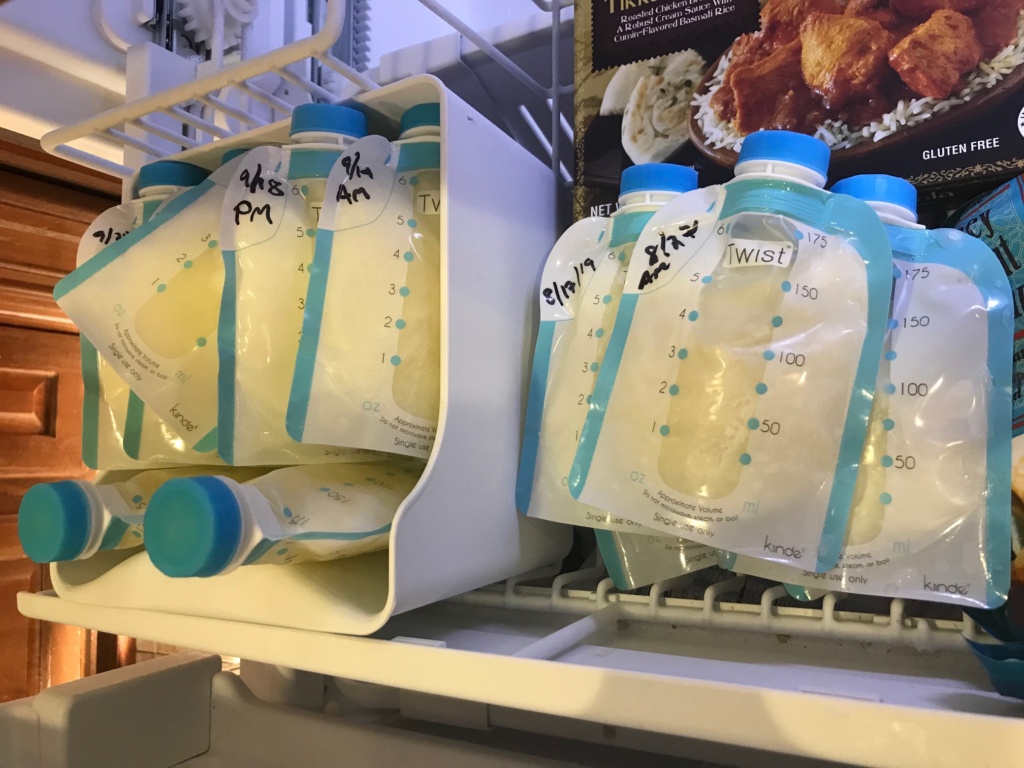
The Governor of the State of California announced late last night a statewide ban on public gatherings and more and more agencies are implementing telework policies that allow employees to work from home. Universities throughout the nation are moving toward online classes and almost all conferences are being canceled / postponed to a later date. Major music festivals such as Coachella and major sports such as the NBA are being suspended. The impacts of COVID-19 are widespread. I commend the decisions in most of these cases to minimize the spread of disease, especially the move of computer work to an online environment. I have always been a proponent of telework, even in a blue skies environment, particularly after becoming a mother. So many people work in industries that are almost entirely computer based and don’t actually require in person interactions at all. So why do we still get in our cars everyday and drive to an office, making traffic just a little bit worse? I think that the widespread usage of telework in response to COVID-19 may enlighten agencies that telework can be a feasible option that actually increases productivity and boosts employee morale (and people will see how much this helps traffic in urban areas!). Especially as a breastfeeding mother, the ability to directly nurse throughout the day would actually increase my working hours as pumping, washing bottles, and properly storing and rationing breastmilk is significantly more time consuming than nursing.
Today, anyone who can definitely should try to complete their work in a place of relative isolation. Those of us who are young and relatively healthy may not see this as imperative, but if it slows the spread of this disease that could be fatal to our elderly families and immune comprised peers (including pregnant women!) then it is certainly worth it. I believe we will find that many of the in person meetings we previously held may have been a drain on resources and will be shorter and more efficient if conducted in an online environment—either through video conferencing, phone calls, or email exchanges.
However, the move toward online work will inevitably leave behind many hourly workers who typically earn lower wages than their salaried office counterparts. Even though the disease does not discriminate based on wealth and fame, as we have already seen with Tom Hanks, politicians, and NBA players being impacted, exposure will almost certainly be disproportionate. In line with so many other disasters, this outbreak will impact socially vulnerable groups, particularly low income populations who already struggle day to day. These are the folks who most often work in customer service roles at gas stations, grocery stores, as hotel maids, as servers in restaurants. Often they don’t have paid sick leave, and shifts may even be canceled due to event cancelations as many aren’t represented by unions to guarantee a set number of hours. These are the people we need to consider and support as a community to ensure that they feel financially secure enough to stay home if they are sick and feel able to care for family members who may be sick. I am fully supportive of extending government paid sick leave for these purposes. We need to think through how we can best protect these workers and how we can sustain these functions with as little human exposure as necessary. I think we need to be innovative now and rise to the challenge of public health to protect all citizens not just those privileged enough to be able to work from home.

Health is Precious
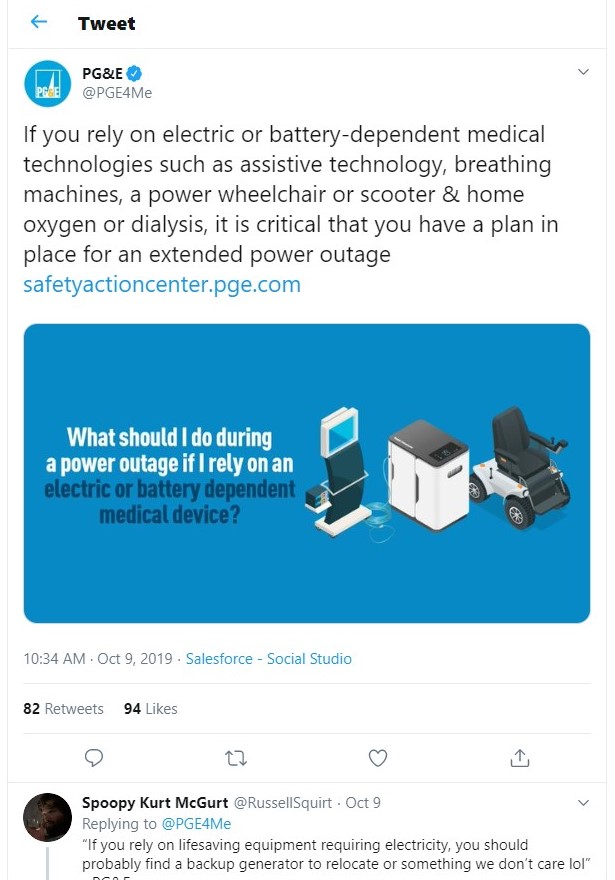
With my daughter starting day care recently and immediately being stricken with a tough cold that had her home for a week and the anxiety of a recent personal health scare, the subject of health was already at the forefront of my thoughts. But now that COVID-19 has so rampantly run through our society, we need to rethink health as a priority. Every day, healthy people take for granted their ability to breathe, to walk, to eat without pain or difficulty. But this status can change rapidly at any moment, especially with such a highly contagious disease that is now so prominent worldwide. This is another way that COVID-19 will have disproportionate impacts, in this case on those who are already challenged by underlying medical issues. We need to take actions to boost our health and our immune systems and to actively be thankful when are well. Far too many of us only think of and wish for health when we are already sick. Instead, I challenge you to be mindfully thankful for your health every day—take pride in heathy choices that you make, eat your veggies, go on that walk, do that yoga, drink that water, EmergenC and green tea! Wash your hands, stay home if you can and remember that if we can slow the spread of this disease we can diminish the immediate need for finite resources such as hospital beds and ventilators, giving older people and those with compromised immune systems the best chance to fight this illness.

Technology and the Culmination of Couch Culture
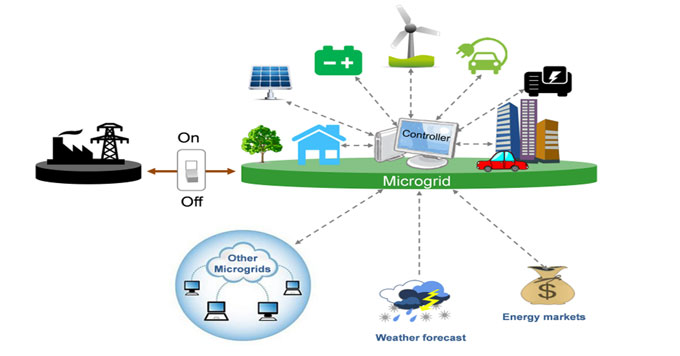
I just recently returned to work after a 7 month maternity leave, some of which I didn’t have a personal vehicle. I am well practiced at social isolation and one of the major factors that makes me feel empowered to stay home is technology. Particularly the plethora of readily available delivery services—I am a regular user of Amazon Prime, Uber Eats and Vons grocery delivery. All of these were not available with the speed and precision just 5 years ago and are still not as accessible in many rural parts of the country. These technologies are a very powerful weapon in the fight against COVID-19 and I think we should make ready use of them. There is no need to make a rush on Costco or Walmart when you can have the essentials brought to your door step. I am aware that there are humans involved in these logistical processes, but I guarantee there are far fewer total opportunities for exposure in the quick interaction of the exchange at the doorstep then there are if you went to a crowded store or restaurant and spent an hour there. As technology progresses, it’s possible to envision a future where we could utilize drones and other automated technologies such as autonomous vehicles rather than Ubers to further mitigate the spread of this biological threat. It goes without saying that the Internet, smart phones, and tools such as Zoom and Go To Meeting are huge technological enablers in the work from home revolution. I know that loss of some hourly jobs is inevitable as we lean more heavily on technology, but I believe there will be more opportunities for creative, strategic employment for the next generation who, like my infant daughter, are practically born with a knack for technology. And isn’t this the perfect culmination of the ‘couch culture’ that we have been cultivating for years?? This generation of 20 somethings goes out far less than prior generations, and who can blame them with so many movies, shows, tasty foods, and even alcohol available with a few swipes of the smart phone? We have already been training for social isolation, now it’s game day.
These are my immediate musings on COVID-19, as I enter a week long period as the Emergency Management Duty Officer for eleven counties in Southern California. In the first nine hours of my shift I have received ELEVEN proclamations of local emergencies for cities and counties in CA. Wish me luck as I attempt to stay on top of this dynamic situation, and feel free to share the thoughts this pandemic is triggering for you.